Almost all animals have some form of visual structures for creating imaging from waves of light. Here are some facts…

Almost all animals.

ContactsDirect ContactsDirect is.

Omega-3s are crucial.
Latest Insights

Your Eyes Are Paying the Price for Online Gambling (Here’s How to Protect Them)
Position your screen at arm’s length and slightly below eye level to reduce strain during extended sessions at table games at Moonbet or other platforms. Every 20 minutes, look at something 20 feet away for 20 seconds—this simple rule helps your eye muscles relax and prevents the fatigue that comes from fixed-distance focus on cards, slots, or live dealer interfaces.
Adjust your screen brightness to match your surrounding environment rather than using maximum settings. Dim lighting creates harsh contrast that forces your eyes to work harder, while overly bright screens in dark rooms cause…

CBD Gummies: A Clear-Eyed Look at Vision Health Benefits
Emerging research reveals CBD’s promising potential for protecting and enhancing eye health through multiple mechanisms. As a natural compound derived from hemp, CBDNorth and other high-quality CBD products have demonstrated anti-inflammatory and neuroprotective properties that may benefit various aspects of ocular health. From reducing intraocular pressure in glaucoma patients to protecting retinal cells from damage, CBD’s interaction with the endocannabinoid system offers exciting possibilities for maintaining optimal vision. While clinical studies are still …

CBD Oil for Glaucoma: What Science Really Says About Eye Pressure
Groundbreaking research reveals CBD oil’s potential as a complementary treatment for glaucoma, offering hope to millions affected by this sight-threatening condition. While traditional glaucoma medications remain essential, studies suggest that CBD’s neuroprotective properties – similar to those found in CBD oil for dogs Canada – may help reduce intraocular pressure and protect retinal cells. However, the relationship between CBD and glaucoma is complex, requiring careful consideration and professional guidance.
Recent clinical trials have demonstrated …

Using CBD For Eyesight? – The Blind Spots to Avoid
Cannabidiol (CBD) comes from the hemp plant. It’s legal and doesn’t make you feel the 5’high’ ingredient found in cannabis. In the United States, more and more people are becoming interested in it. While there are concerns like CBD causing red eye, people who support CBD talk about all the good things it can do for your health. They claim it can help with anxiety and make seizures happen less often in people with epilepsy. People also believe you can use CBD for eyesight.
Some folks also think CBD can …

Ultimate Guide to Mowing Goggles – Choosing, Using, and Maintaining Your Eye Protection
Mowing the lawn, a routine chore for many, is not without its risks, especially regarding eye protection. Amidst the hum of lawnmowers and the scent of freshly cut grass lies the potential danger from flying debris and dust. In this context, mowing goggles are crucial personal protective equipment.
While often overshadowed by more conspicuous tools like gloves or a dust mask, these goggles are pivotal in safeguarding one’s vision against particles that lawn mowing can unleash. This article explores the necessity of safety glasses, features, and the …

Vaping Without Blurring: How to Safeguard Your Vision
While there has been much discussion about the potential adverse effects of vaping on various aspects of health, one area that is often overlooked is the impact on vision.
Before you are buying vaping products online, you should look at our tips below that may help you safeguard your vision while enjoying your vaping experience. They’re as follows:
Stay Hydrated
One of the most straightforward and effective ways to protect your vision while vaping is to stay adequately hydrated.
Vaping can cause mild dehydration which can lead to dry eyes…
How Your Health can be Shown by Your Eyes
Here are some health conditions that can be detected based on how your eyes look:
Diabetes
Diabetic retinopathy affects the retina capillaries. It is among the causes of blindness in most American adults. Symptoms such as eye pain, floaters, and blurry vision may not appear or get detected until the condition exacerbates, making routine eye exams essential. An eye doctor may detect signs of diabetic retinopathy before a diabetes diagnosis and allows early lifestyle changes and treatment.
High Cholesterol
Arcus senilis is a white, gray, or blue ring that can form around the iris due to cholesterol build-up. …

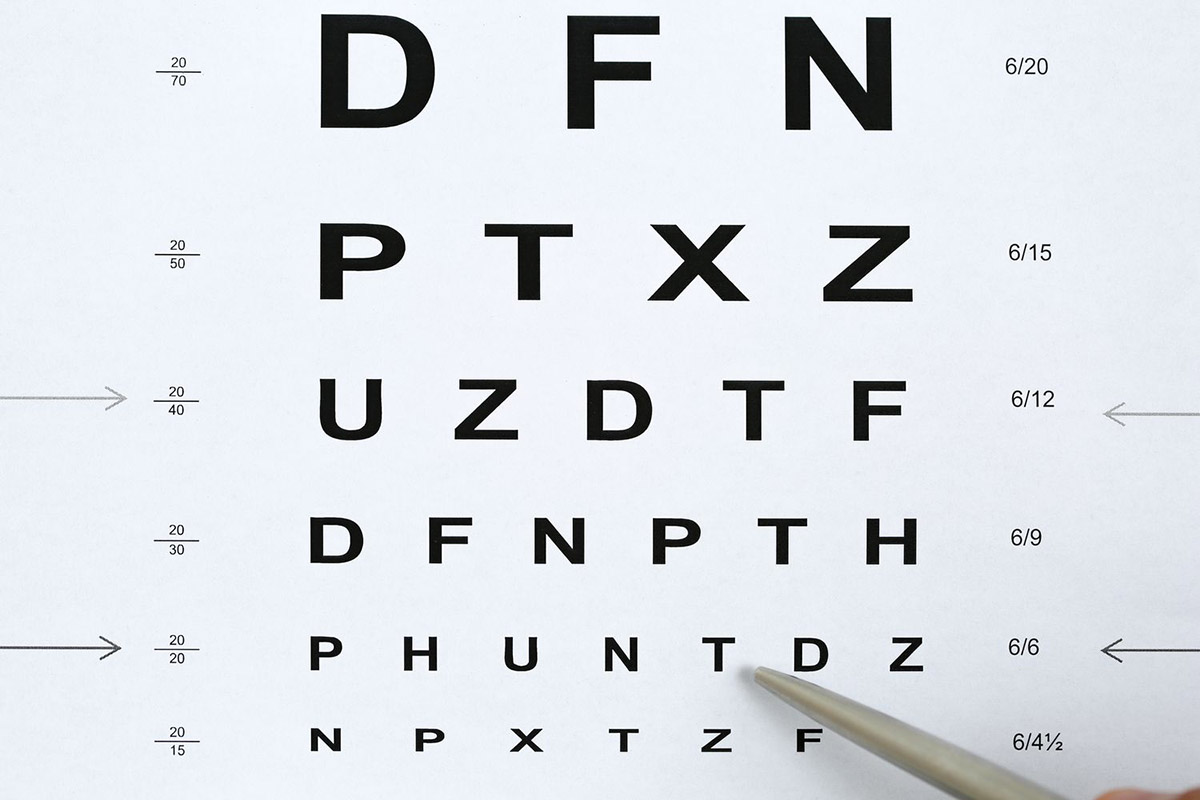
Definition of Legally Blind
Being legally blind means a person’s vision is 20/200 or worse even with corrective lenses. It’s different from low vision, which is 20/70 or worse even with correction. Impaired vision and vision loss refer to reduced sight that causes difficulty in daily activities.
Legal blindness can be partial, meaning there’s a partial loss of vision in one or both eyes. It can also be total, where there’s complete vision loss in both eyes. Blindness can be caused by cataracts, glaucoma, or retinopathy.
BrailleBug is an educational site that offers braille games and resources for children, parents, and teachers …